Activity
Click here to see the Assignment
Michael Kaufman: I’d like to hear about the conversations you’ve had.
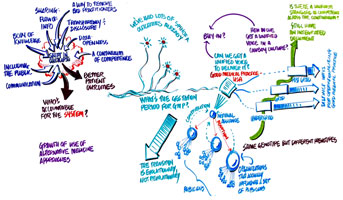
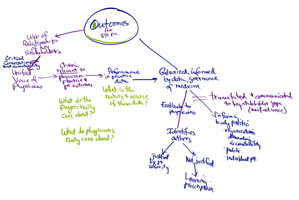
Accountability. Some of the things we talked about is who is accountable for the system, especially in third-party payors, and how accountability is determined.
We’d like to know what the gestation period is for the Good Medical Practice document.
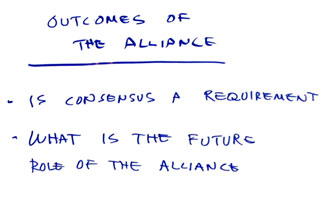
If we can get together as a unified force, then we can determine when it’s done. We cannot be paralyzed by having no governance of this group and our process.
MK: Those are big things you’ve just said. You are the people who can make those decisions.
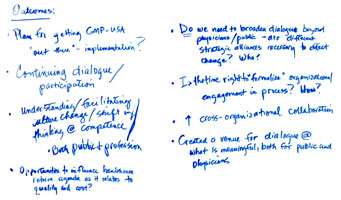
Each of the various stakeholders needs to look at the GMP from a slightly different perspective to understand how to operationalize it. Might we get to a point of delivery sooner if we were to have these answers and then link the answers to each other?
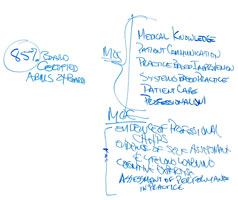
MK: We’ve talked about the continuum of competence. If I understand correctly, you’re saying that every stakeholder group needs to have their own translation and their own application of the GMP, right?
Right.
We’re a cottage industry and believe in it, so we have to be able to do our own thing. We need a change in culture in order to adopt this kind of a system.
The undergraduate group would have a distinct way of operationalizing it compared to the post-graduate group. The issues of vertical versus horizontal integration in the curriculum are the same and regardless of your dominant mode, you have to find a way to integrate the other way. I don’t think our method should be helter-skelter, but we might be better off solving the issues individually and then linking them.
We looked at increasing skill-sets. One thing the summits haven’t wrestled with is how to develop competency within the depths of the specialties.
MK: One of the reasons that the summit dialogues have continued is because we don’t have a definition that is shared across any of these groups. It is also possible the definition is changing. This group is determining the definition today - which is different than what it was yesterday. You can see it either way: that there is a way of measuring competence has a single right answer and there’s nothing else to do. Another way is to understand that there is a right answer in any given moment which changes. This group is exploring this.
If you follow the dollars, the most rapidly increasing expenditures are in the alternative medicine field in which we have no control over, not in the traditional areas.
We’re used to the aggregate voice, but we’re a cowboy culture. What would it take to motivate us to care about the other areas? Does the profession as a whole care about this and what could we do to motivate them?
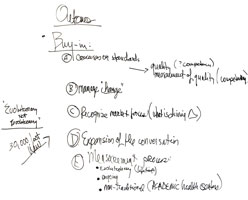
How do you get buy-in from the practicing physicians? If a distant national organization comes out with a pronouncement, a practicing physician isn’t going to pay attention, but if someone close, like someone in their state or specialty society endorses something, they’re more like to buy-in to it. We need to get down to the local physicians.
MK: We call that a transition strategy. The question I posed relates to the need for outcomes. We know that if we all sign our names to an outcome and leave it there, it won’t mean anything. From there we have to figure out how to transition, but I’m not sure we’re there yet.
Do we have to have an outcome? Or can we just say that there will be a monitoring group and the rest of the agencies are required to follow through on that? GMP is the outcome.
At the 30K foot view, we’re talking about how we manage change. This is not revolutionary, but evolutionary and we need to figure out how to make that happen.
Our group looked at it differently. The outcome of this group should be what occurs through the training. We thought hard about systems that work and we teased apart the characteristics of those systems. There’s a partitioning of a body of knowledge with a free-flow of information, transparency to all parties, and a sense of openness and sharing of data. For us this would require a cultural change to incorporate those qualities.
We talked about our concerns that were implied in the questions. The spin-offs that have come from the discussions are very rich in terms of outcomes. No one knew about all of them or even the majority of them. When we talk about what happens in the future, maybe this is the think tank that brings the right people into the room? Maybe we need to invest in that and we should look at what has happened outside these meetings so that more of us are aware of what’s going on.
Patty Skolnick: I lost my child 4 years ago due to an unnecessary surgery performed by a surgeon who had malpractice in his history. When I researched this man I found nothing that looked out of place. I left my job in corporate America in order to address this issue. I applaud what you’ve done and what you’re doing. I’ve been all over the country and have talked to many people including medical students and doctors. You are all talking about the most important things. Maybe some of you have lost a child. It was my only child. I want to thank each and every one of you for what you do and for being brave enough to come here whether your organizations agree with you or not. This is a journey that I never thought I would be on but you’re so on the right path.
Question: What outcome would you like to see?
PS: One would be that physicians would share what’s going on with each other, transparency and disclosure so that the public can make informed decisions in choosing their medical provider. We would like to see that there is a continuum from medical students to residents to practicing physicians to make sure their standards are up to par, and to ensure that the bad apples go away. If someone does things repeatedly wrong, they need to do something else. Communication is essential. Patients need to be participants in their own healthcare and need to be respected when they ask questions. The neurosurgeon had the ‘you’re just the mom’ syndrome and it influenced the way he interacted with me.
Question: Most of us operate within a system of care. We don’t operate within a silo. How do you see this impacting what you’re talking about? This is team medicine.
PS: I see it as one person at a time. My biggest pleasure is talking with 4th year medical students and hearing them say that we’ll be better doctors. I didn’t go to scare them but just to help them understand what position they’re in. The more we talk to one another, the better we’ll all do. I started out on the legal end. The insurance company wanted to settle right away and I told them I don’t want the money, I want justice. I want to ensure that this doctor cannot practice ever again. I sat through a 5-week trial and saw that they put a mom through a terrible experience instead of just taking care of the problem. I found out at the deposition that another surgeon even said as he was scrubbing up that he didn’t know why he was doing this surgery. My 22-year old nurse student, a vet tech, a kid that had come full circle after a tough life, lost his life by a doctor who had malpractice in 3 other states. His 3-hour surgery took 6-hours. His one week stay in the hospital turned into a 6-month ICU stay. He was in a coma and had every infection you can imagine. This doctor told me he’d be fine and I believed him. It almost broke up my 35 year marriage. We the public believe because we want to. We want to believe that doctors are doing the right thing. We also believe that the agencies that ensure competency are working. I want you to know that this doctor is still practicing. I was offered $3M. This doesn’t make any sense. We’re going to do whatever we can to make a difference in Colorado and hopefully throughout the country.
MK: I have nothing more to add. Thank you all for coming. We will see you in the morning.


Scribing
Click on a thumbnail below to open the full size image in a new window


Work Walls