
Health care is of course a topic of great interest and concern globally, as the confluence of macro factors have converged to make it one of the most significant issues facing leaders and citizens in all nations.
As we are all aware, advances in diagnosis and treatment are coming almost daily, as new approaches and technologies are developed. But many carry with them high costs, and health care is consuming an ever greater portion of national GDP around the world. This is on top of the fact that access to health care is very uneven within and among countries, highlighting profound inequities.
To address this issue, the World Economic Forum has just published a new white paper entitled
Global Future Council on Health and Healthcare 2018-2019
A Vision for the Future: Transforming Health Systems
The report studies five diseases in five countries, compares the current situation with the ideal for 2030, and suggests policy initiatives to improve both access and equity.
Among the key findings
From the Introduction: “Health systems are under major pressure globally. Population growth, ageing, the emergence of personalized medicine and the growing potential of new technologies, along with rapidly rising costs and the entry of disruptive and non-traditional competitors, will increase demand for services and affect the performance and sustainability of healthcare delivery systems. By 2050, one in six people will be over 65 years old1 and more people will live with one or more chronic diseases. Despite reforms in funding and payment models in some countries, there is ample evidence of waste and inefficiencies in health systems.2 Global healthcare spending is projected to continue increasing.” (Page 5)
And from the Conclusion: “A societal transformation towards healthier lifestyle choices is needed, together with several other actions: a re-engineering of health systems to put people at the centre, the provision of adequate funding which ensures that money is well spent, and a culture of building partnerships to deliver good outcomes. This also means having the right global health architecture and the support from legislators for the necessary legislation and budgets at the national level, as well as leadership from communities and action across government to ensure the design of health systems that leave no one left behind.” (Page 22)
InnovationLabs participated in the preparation of the report by conducting a study of breast cancer in the US. We conducted in-depth interviews with women who have had breast cancer, their caregivers and clinicians, and with health care policy makers.
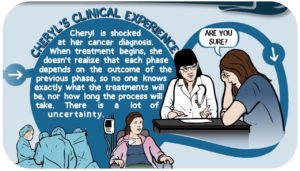
As reflected in the WEF report, we found that the treatment journey for many women is a long and difficult one. We learned that the course of treatment can be different for each patient depending on the type of cancer they have, and their specific genetic and metabolic characteristics. Consequently, a clinician may not know at the outset of treatment what the actual course of treatment will be, presenting another dimensions uncertainty that naturally adds fear and anxiety for patients who are already extremely stressed.
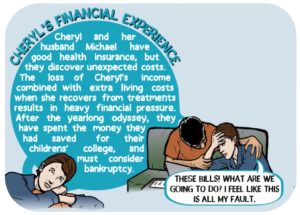
In addition, even those who have good health care coverage often find themselves with unexpected costs while at the same time enduring a loss of income during treatment periods when they are simply too sick to work. Medical bankruptcy is thus far too common in the US, even among those with health insurance.
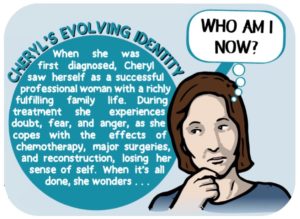
During the course of their long and difficult treatment periods, many women also find that their sense of self is lost, and they experience an identity crisis even when treatment is successful and they are cancer free.
This difficult journey is summarized in the graphics below, which was prepared by the exceptionally skilled Christopher Fuller of Griot’s Eye.
You can see more of Christopher’s work, and read some of his insights on the graphic arts at his very fine web site.
The vision for 2030 as articulated in the WEF paper suggests the need for significant improvements to care, as well as better and much more equitable access. Nine policy initiatives were identified to help achieve these goals:
- Work in partnerships across sectors to design the health systems of the future.
To provide the best possible health outcomes for populations by 2030, policy-makers, industry leaders, academia, members of civil society and practitioners must work closely together to reorient health systems to become people-centred and holistic.
- Address the social determinants of health and health inequalities.
To ensure that people stay healthy, it is essential to address these wider social and economic conditions affecting health in addition to providing adequate quality, people-centred health services.
- Prioritize and support universal health coverage, including through appropriate human and physical resources.
Access to basic services should be recognized as imperative, supported by focused budget allocations and an emphasis on the quality of services.
- Increase the focus on preventing disease and promoting health.
Type 2 diabetes and heart disease are two examples of diseases whose incidence could be both significantly reduced and better controlled with effective regulation and access to better nutrition and exercise. Prevention and early detection should be supported across all generations – from birth to advanced age.
- Strengthen primary healthcare.
A robust primary care sector is the linchpin of good health services and should be a priority for national and international health agencies. It increases access to care and helps many people stay as healthy as possible during their lifetime by providing immunizations, antenatal care and chronic disease management.
- Empower and engage people and their communities.
Staying healthy also requires actions and choices by individuals and their families. Communities can complement government policies and programmes that assist individuals to stay healthy, such as by providing access to the right information and improving health literacy. Changing lifestyles requires a package of policy approaches that affect individuals, populations and the landscape where they operate.
- Promote people-centred innovation and technologies.
The Fourth Industrial Revolution will provide a platform for bridging the gaps between people of different locations and milieux. Bringing the human touch and sophisticated technology together in seamless patient journeys, deployed locally, will make care accessible to many. Big data and analytics have the potential to provide better ways to evaluate individuals’ outcomes and cut across silos of care.
- Allocate the appropriate resources to health and social systems and maximize value for money.
Governments need to create enough fiscal space to sustain a minimum level of public investment in essential health services and to minimize impoverishing households through out-of-pocket expenses.
- Promote accountability and leadership.
Achieving this vision requires strong accountability mechanisms (application of laws, regulations, ethical standards and norms) throughout the health system. Leadership and policy alignment are needed to accelerate new solutions and engage providers, payers, employers and staff, and patients and their families towards an accountable, more efficient and transparent health system.
For each of the five scenarios covered in the WEF report, the future state vision for 2030 suggests great opportunities to make the world a healthier and more equitable place for us all.
Overall, the transformation of health care systems globally presents a huge challenge to our social, cultural, and economic systems, and it is through efforts such as these that we will uncover the necessary insights and commitments to address them.
Our thanks to WEF and its US affiliate Kaiser Permanente for inviting us to join in this important work. Thanks also to Julie Busch of Product Rehab for her fine work on this project!
We welcome your feedback, as always.
Thanks!

